Understanding Obesity as a Brain and Hormone Disorder
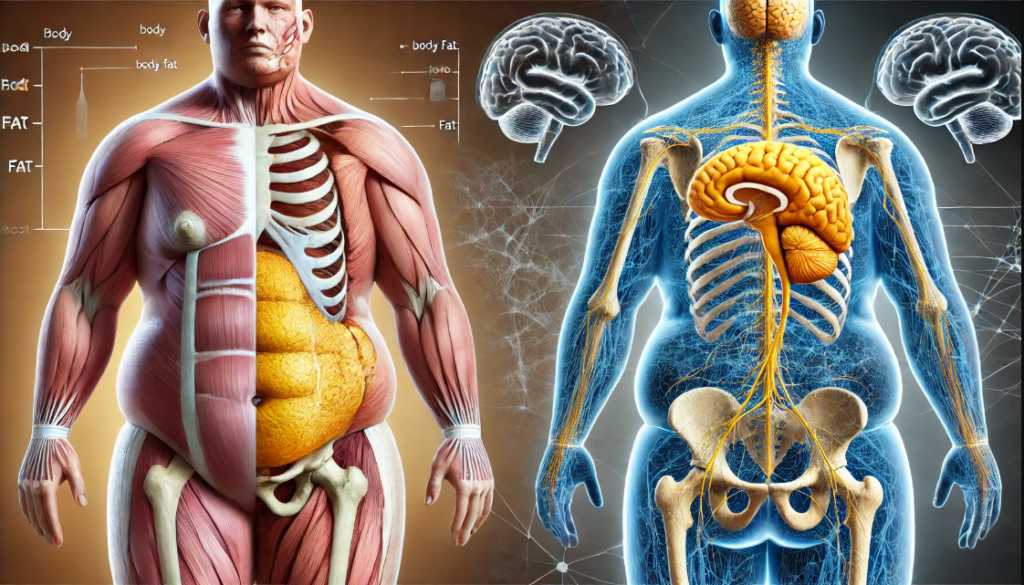
Hey there! Let me tell you something interesting about obesity. You see, obesity is one of the most common health issues worldwide. We often think it’s just about eating too much and not moving enough, but it turns out, it’s a lot more complicated than that. Recently, scientists have been looking at obesity as a disorder that involves both our brain and our hormones.
So, what exactly is obesity? According to the World Health Organization, it’s when there’s an excessive amount of fat in your body that can harm your health. They use something called the body mass index, or BMI, to measure it. If your BMI is between 30 and 34.9, that’s considered Grade I obesity. Between 35 and 39.9 is Grade II, and anything over 40 is Grade III. In 2016, about 13% of adults worldwide were obese—that’s 650 million people! In some places, like Mexico, a whopping 36% of adults are obese.
BMI is just your weight divided by your height, but it does no differentiate if your weight is muscle, fat, bone, etc.
Now, let’s talk about how our brain and hormones control our appetite. There’s this part of the brain called the hypothalamus that gets signals from various parts of our body, like our fat tissues, digestive tract, and pancreas. These signals help us figure out when to eat and when to stop. There are two main systems at play here: the homeostatic system and the hedonic system.
The homeostatic system is all about eating to survive. It includes hormones like leptin and insulin, which tell us when we’re full and when we need more energy. On the other hand, the hedonic system is about the pleasure of eating. This system is controlled by a circuit in the brain that makes us crave certain foods, enjoy them, and sometimes overeat.
But wait, there’s more! There are several other factors that contribute to obesity. For example, our genes and how they change over time can influence how our body handles energy and stores fat. Then, there are environmental factors. Think about it—easy access to high-calorie foods, a sedentary lifestyle, stress, and long working hours can all increase the risk of obesity. The bacteria in our gut, known as the microbiota, also play a role in how we digest food and store fat. And get this—high-fat diets can cause inflammation in the brain, which messes with how hormones like leptin and insulin work.
Why is this so important? Well, obesity doesn’t just make it harder to move around. It increases the risk of many serious diseases, like heart problems, diabetes, breathing issues, and even some types of cancer. Plus, it can affect our mental health, leading to depression and anxiety.
So, what can we do about it? To tackle obesity, we need to take a comprehensive approach. It’s not just about eating less and exercising more. We also need to manage stress, get enough sleep, and improve our environment to support a healthier lifestyle.
In conclusion, obesity is a complex disease that involves much more than just calorie intake and expenditure. By understanding how our brain and hormones influence our eating habits, we can develop better strategies to treat and prevent obesity. Ongoing research in this field is crucial for finding effective solutions that improve people’s health worldwide.
Reference
Ferreira-Hermosillo, A., de Miguel Ibañez, R., Pérez-Dionisio, E. K., & Villalobos-Mata, K. A. (2023). Obesity as a Neuroendocrine Disorder. Archives of Medical Research, 54, 102896. https://doi.org/10.1016/j.arcmed.2023.102896.